Clinical medicine of today is complemented with biological markers which help not only in diagnosing, prognosticating but also monitoring the efficacy of the treatment being given. According to WHO their measurement may be bio-chemical, physiological, cellular or molecular.
There are numerous novel bio-markers in various medical specialities. Currently intensive work is going on for the development of innovative, more effective and acceptable bio-markers.
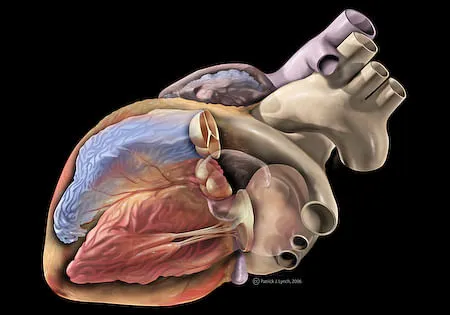
Important Bio-markers for Cardiology:
1 For acute coronary syndromes (Unstable Angina and Heart Attacks)
Chest pain is a very common symptom which brings patients for medical attention often in hospital emergencies and also to doctor’s clinics. In this situation diagnosing of a cardiac pain due to blockage of a coronary artery is extremely important and should be done at the earliest. Electrocardiography is very useful if it is a full-fledged heart attack called ST elevation myocardial infarction (STEMI). These patients need immediate care in a cardiology centre or a specialized medical unit capable of administering clot busting drugs (Streptokinase or Tenecteplase etc).
However, at least 50% of heart attacks do not have a tell-tale ECG change, yet they have a partial blockade because of a clot in the heart artery. These are the patients where bio-markers are very useful.
Markers of Myocardial Damage:
CPK and CPK-MB
Creatine kinase (CK) and creatine kinase-MB (CK-MB) have a long history as the gold standard for acute myocardial infarction (AMI) diagnosis. CK-MB is a CK isoenzyme, predominantly found in the myocardium. Its elevation occurs 4–6 h after the onset of injury to the heart and remains so for 24–48 h. Higher is the level, more is the damage.
Cardiac Troponins (Trop t and Trop i)
Cardiac troponin T (cTnT) and cardiac troponin I (cTnI) are more sensitive and specific markers than CK-MB in detecting myocardial necrosis, and have become the preferred biomarkers for the diagnosis of AMI. They are also a useful prognostic indicator in patients with ACS. The superior clinical performance of troponin results from its higher sensitivity for smaller myocardial injury and is considered the gold-standard in the new definition of heart attack. These markers can be used as a qualitative method showing positive or negative using a strip needing a drop of blood. An extra line coming within a few minutes indicates damage to the heart muscle. However, this method does not give the quantitative value. Quantitative values are important in getting the information regarding the severity of the muscle damage. Higher values are accompanied by more complications.
Natriuretic Peptides (BNP and nt Pro BNP)
These peptides are released from the heart tissues in response to stretch of the muscle and are activated in heart failure and related conditions. A large heart attack results in weakening of the heart muscle and can lead to its increase. This is a very useful marker in heart failure diagnosis but also prognosticates ACS patients .
C Reactive Protein (CRP)
CRP is the most widely studied inflammation marker. CRP is an acute-phase protein and a marker of inflammation. Heart attack is always associated with variable degrees of inflammation. A high CRP beyond 3 units means active inflammation. However, it is very non-specific and can be high in many conditions associated with inflammation. The classical example is that its values used to be very high in the recent COVID pandemic. Simplicity in estimating it is a big advantage. As such its value is when done along with troponin estimation, a high level adds to the diagnostic power and prognosis.
Although use of multiple bio-markers is theoretically attractive, however there is no evidence that a strategy based on measurement of more than two markers (besides troponin and CRP or natriuretic peptides) improves the diagnostic and prognostic power. So far, indeed, consistent and reliable data on diagnostic and prognostic value of these markers are available only for Troponin, BNP and CRP.
Further studies are need to establish the role of several new biomarkers which are available in the clinical practice of diagnosing and managing heart attacks.
2. Biomarkers for Heart Failure:
The role of biomarkers in heart failure (HF) is being increasingly utilized. These cardiac markers are used as simple methods to assess the status of a patient with HF along with the possibility of monitoring changes induced by the treatment. Biomarkers can be used to assess to a variety of pathophysiological processes responsible for the occurrence of HF. These tests also help to identify a patient’s response to a particular treatment regimen.
Natriuretic Peptides (NP’s)
A number of peptides have been described: atrial natriuretic peptide (ANP), brain natriuretic peptide (BNP), C-type natriuretic peptide etc. In clinical monitoring most attention has been directed at BNP and N terminal pro-BNP (NT-proBNP). These biomarkers are peptide hormones synthesized by the heart but also by other organs. NP’ s are the most extensively studied biomarkers that have been used in HF management. As a result of the stretch of the heart muscle the gene coding for BNP is activated and the pro-hormone pro-BNP1 is produced.
The latest international guidelines recommend the measurement of NP’ s to provide assistance in the diagnosis of HF in suspected patients. Levels of NPs should be measured as an initial diagnostic test, especially in the non-acute setting, when echocardiography is not immediately available. Indeed, increased plasma levels may help identify patients who need further cardiac investigation. Also, NPs along with troponins (trop t) can be used to identify patients at higher risk and may be helpful in monitoring the use of newer drugs.
In a patient with severe shortness of breath of uncertain cause the estimation of NP’s immediately helps in differentiating respiratory cause from a cardiac cause. The management of these two conditions is often entirely different. Newer agents for managing heart failure like Sacubitril/ valsartan combination (Vymada) under the guidance of nt Pro BNP is the way to go. With the start of treatment reduction in the values, indicates its efficacy.
Troponins in HF:
Measuring high sensitivity troponin in patients at risk of HF has been found to provide additional predictive value. For these reasons, increased levels of troponin have prognostic value for poor outcomes in both acute and chronic HF. Important studies have shown increased cardiac troponin to be an independent predictor of in-hospital mortality. Subsequent studies have confirmed the presence of high levels of troponin in acute HF patients to be associated with higher risk of dying.
As per the international guideline’s troponin estimation is a very important test in patients with heart failure needing hospitalization. It is also an important part of the diagnosis of ACS and may indicate the cause of heart failure in some situations. The routine measurement of this in HF patients may not however add to the improved outcome of these patients.
St2 (Soluble suppression of tumorigenesis-2 Suppression of tumorigenesis-2.
This marker is being increasing utilized in patients of HF. Elevation of this bio- marker indicates problems of the heart muscle beyond what can be got from nt Pro BNP and troponin estimation. Soluble ST2 (sST2) is known to be a marker of inflammation and stress on the heart muscle. It is a very strong predictor of adverse clinical outcomes within a HF population. Its elevation beyond the cut off limits indicates poor outcome and alerts the doctor to manage the patient aggressively. These patients often improve by the addition of a group of drugs like spironolactone.
Multi-marker approach in Heart Failure management:
There is evidence that this combined strategy leads to improved measurement of HF risk compared to traditional risk scores. A multiple score composed of several biomarkers provides the more reliable prognostic value compared to any single biomarker strategy. Thus, combining biomarkers may improve the ability to predict the prognosis. Beyond natriuretic peptides and cardiac troponins, soluble ST2 may be indicated to aid in the diagnosis and in predicting the prognosis of the patient with heart failure.
Take Home Message:
Biomarkers are of great utility in managing the patients of heart attacks and heart failure. Routine use of these along with repeating during follow up is the best way of optimizing the management of these patients and improving their outcomes. Their use should increase and physicians must know their importance in contemporary medicine.
Disclaimer: The views and opinions expressed in this article are the personal opinions of the author. The facts, analysis, assumptions and perspective appearing in the article do not reflect the views of GK.
Prof Upendra Kaul is a renowned cardiologist and founder Director, Gauri Kaul foundation. Recipient of Dr B C Roy Award and Padma Shri.